Background and purpose: Degenerative change of the corpus callosum might serve as a clinically useful surrogate marker for net pathological cerebral impact of diabetes type 1. We compared manual and automatic measurements of the corpus callosum, as well as differences in callosal cross-sectional area between subjects with type 1 diabetes and healthy controls.
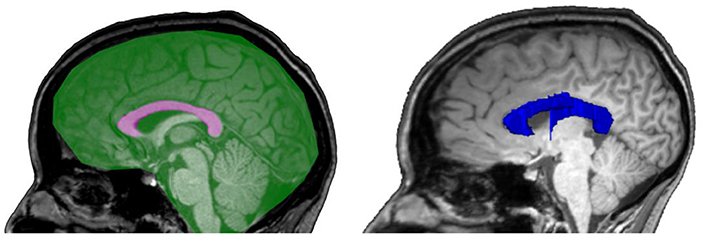
Materials and methods: This is a cross-sectional study on 188 neurologically asymptomatic participants with type 1 diabetes and 30 healthy age- and sex-matched control subjects, recruited as part of the Finnish Diabetic Nephropathy Study. All participants underwent clinical work-up and brain MRI. Callosal area was manually measured and callosal volume quantified with FreeSurfer. The measures were normalized using manually measured mid-sagittal intracranial area and volumetric intracranial volume, respectively.
Results: Manual and automatic measurements correlated well (callosal area vs. volume: ρ = 0.83, p < 0.001 and mid-sagittal area vs. intracranial volume: ρ = 0.82, p < 0.001). We found no significant differences in the callosal measures between cases and controls. In type 1 diabetes, the lowest quartile of normalized callosal area was associated with higher insulin doses (p = 0.029) and reduced insulin sensitivity (p = 0.033). In addition, participants with more than two cerebral microbleeds had smaller callosal area (p = 0.002).
Conclusion: Manually measured callosal area and automatically segmented are interchangeable. The association seen between callosal size with cerebral microbleeds and insulin resistance is indicative of small vessel disease pathology in diabetes type 1.
Reference: Claesson T, Putaala J, Shams S, Salli E, Gordin D, Liebkind R, Forsblom C, Summanen PA, Tatlisumak T, Groop P-H, Martola J and Thorn LM (2020) Comparison of Manual Cross-Sectional Measurements and Automatic Volumetry of the Corpus Callosum, and Their Clinical Impact: A Study on Type 1 Diabetes and Healthy Controls. Front. Neurol. 11:27. doi: 10.3389/fneur.2020.00027